Attention, fellow humans! It’s time to chill out… literally! 🧊
Our bodies are on a cosmic cooldown, and it’s not just because we’ve all become walking popsicles addicted to air conditioning. Oh no, this is far more sinister and hilarious than that!
The Great American Refrigeration❄️
Since the 1800s, our core temperatures have been dropping faster than a clumsy thermometer. We’re talking a whopping 0.02°C every decade! That’s right, we’re slowly turning into the most disappointing soup ever. But wait, there’s more! Since the 1960s, we’ve kicked it up a notch (or should I say, down a notch?) to 0.03°C per decade. At this rate, by the year 3000, we’ll be walking icicles with a pulse!
Why Are We Becoming Human Popsicles? WE CAN ONLY SPECULATE… 🤔🍦
Evolution’s Cruel Joke: Mother Nature decided humans were too hot to handle and is slowly turning us into the world’s most disappointing reptiles.
Alien Invasion Prep: The lizard people are gradually lowering our body temperature to make Earth more hospitable for their impending arrival. Wake up, sheeple!
The Great Air Conditioning Conspiracy: Big AC has been secretly lowering our tolerance for heat. Soon, we’ll need climate control just to survive a mild spring day!
Revenge of the Ice Age: Those woolly mammoths we hunted to extinction? Their ghosts are getting the last laugh by slowly freezing us from the inside out.
Metabolic Mutiny: Our bodies have unionized and are going on a perpetual energy-saving strike. Lazy mitochondria, unite!
hYPOTHERMIA AND modern plagues 🥶
Let’s break it down, shall we? As our core temps plummet, we’re inching closer to hypothermia territory. Remember, folks, anything below 95°F (35°C) is a one-way ticket to Hypothermia Town. And let me tell you, it’s not a fun place to visit.
Early Signs of Hypothermia (The “I’m totally fine” phase):
-Teeth chattering like a wind-up toy on crack
-Fingers so numb you could probably chop them off and not notice
-Sudden urge to cuddle with strangers (or bears, if available)
-Ability to see your breath and mistaking it for a cool new superpower
-Uncontrollable desire to do the “pee pee dance” (even if you don’t need to go)
Medium Signs of Hypothermia (The “Okay, maybe I’m not fine” phase):
-Brain functioning at the speed of a frozen molasses spill
-Muscles stiffer than your grandpa’s arthritis
-Skin turning a lovely shade of “corpse chic” blue
-Speech so slurred people think you’ve discovered a new language
-Coordination rivaling that of a newborn giraffe on roller skates
But wait, there’s more! Our cooler cores might be the secret ingredient in the recipe for modern epidemics. Let’s connect some dots, shall we?
The Common Cold Conspiracy: As our bodies cool, we’re becoming the perfect hosts for those pesky rhinoviruses. They’re throwing parties in our nasal passages, and we’re too chilly to kick them out!
The COVID Conundrum: Could our cooler temps be giving SARS-CoV-2 the VIP treatment? It’s like we’ve rolled out the red carpet for these viral villains!
The Inflammation Invasion: Our dropping temps might be linked to reduced inflammation. Sounds good, right? Wrong! It’s like we’ve fired our body’s security team, leaving us vulnerable to all sorts of microbial mischief!
The Metabolic Meltdown: Lower body temp means a slower metabolism. We’re turning into human sloths, people! Next thing you know, we’ll be hanging upside down from trees and eating leaves.
As for health benefits of lower body temperatures:
-Calorie-burning bonanza: Shivering is nature’s way of giving you killer abs
-Natural botox: Cold temperatures can temporarily freeze those wrinkles right off your face
-Instant ice pack: You become a walking first-aid kit for sports injuries
-Superhuman pain tolerance: Can’t feel pain if you can’t feel anything at all!
These “benefits” are about as useful as a chocolate teapot in a sauna.
So, what’s the solution? Should we all move to the Sahara? Start internal bonfires? Wear seven layers of clothing at all times? Remember, folks, this isn’t just about comfort anymore. It’s about survival! The next time someone tells you to “chill out,” look them dead in the eye and say, “No thanks, I’m trying to avoid the next pandemic!” Stay warm, stay vigilant, and for the love of all that’s holy, check your temperature! 🌡️🔥
Chilling Revelations: Nazi Freezing Experiments That Left Humanity Cold
The mastermind behind this frozen nightmare? None other than Dr. Sigmund Rascher, the SS’s very own Dr. Freeze. This ambitious “rising star” in medical research joined the SS in 1939, proving that some people will do anything for a career boost. Rascher’s experiments weren’t just about seeing how long it takes for a human to turn into an icicle. Oh no, he had grander plans! Rascher reported his findings at the 1942 medical conference titled “Medical Problems Arising from Sea and Winter.” One can only imagine the coffee break conversations at that particular gathering.
And just when you thought it couldn’t get any more bizarre, enter Heinrich Himmler with his… unique… suggestion for warming hypothermic victims. Let’s just say it involved forced “intimate contact” between victims. Because apparently, even in the depths of cruelty, there’s always room for a twisted matchmaker. The scale of this icy horror? A chilling 360 to 400 experiments involving 280 to 300 victims. Some unlucky souls even got to experience the joy of multiple experiments.
While the official narrative focuses on the stated goals of helping German soldiers and pilots, you’d be right to be skeptical. The Nazi freezing experiments were likely about far more than just survival in cold conditions. Some alternative possibilities to consider:
Sadistic curiosity: The experiments may have been a way for Nazi doctors to indulge their most depraved impulses under the guise of “science.”
Pushing human limits: They could have been trying to determine the absolute extremes the human body could withstand, perhaps with transhumanist aspirations.
Torture methods: The Nazis may have been developing new interrogation and torture techniques disguised as medical research.
Cryogenic preservation: There are fringe theories that the Nazis were exploring ways to preserve humans in suspended animation.
Occult rituals: Some speculate these experiments had mystical purposes related to Nazi occultism.
Mind control: The extreme conditions may have been used to break down prisoners psychologically for brainwashing experiments.
Eugenics data: The Nazis could have been gathering data on how different “races” responded to extreme cold as part of their racial ideology.
While we can’t know for certain, the sheer cruelty and scale of these experiments suggest motives far darker than just helping soldiers stay warm. The official explanation may be a sanitized version of a much more sinister truth. In the end, these experiments left not just their victims cold, but the very soul of humanity. As we look back on this dark chapter, let’s remember that sometimes, the most chilling aspects of history aren’t found in frozen water, but in the frozen hearts of those who would conduct such atrocities. Stay warm, folks. And maybe give your thermostat a little hug tonight. 🌡️❤️
Nuremberg: Frost and Furious (The Doctors’ Trial)
Oh boy, buckle up buttercups, because we’re about to dive into the icy depths of Nazi depravity at the Doctors’ Trial! 🥶
Our main man, Dr. Sigmund “Freeze” Rascher, reportedly met a fittingly frosty end before he could even face trial. After his wife’s baby-snatching shenanigans were exposed (turns out, faking pregnancies at 48 isn’t a great career move), Himmler went from BFF to “Bye Felicia” faster than you can say “brrr.” Rascher was shipped off to Dachau, where he was executed on April 26, 1945, just days before the camp was liberated. Around the same time, his wife was reportedly executed by hanging in Ravensbrück. Hm…
The freezing experiments were front and center at the Doctors’ Trial like a twisted episode of “Ice Road Truckers” meets “Law & Order: Third Reich Unit.” This 140-day courtroom drama featured a cast of characters who thought “First, do no harm” was more of a suggestion than a rule. The prosecution at the Doctors’ Trial was all over this like frost on a windshield. They laid out how Rascher and his merry band of psychopaths subjected many victims to these arctic atrocities.
But wait, there’s more! When the victims’ internal body temp hit a balmy 79.7°F, our genius docs tried to “rewarm” them. Their methods? Hot sleeping bags, scalding baths, and – I kid you not – forcing naked women to “copulate” with the frozen victims. Because nothing says “medical science” like non-consensual hypothermic hanky-panky, am I right? 🙄
Now, let’s meet our frosty felons:
Rudolf Brandt: Himmler’s personal paper-pusher. Convicted and got a one-way ticket to the gallows.
Karl Gebhardt: SS’s chief surgeon. Convicted and hanged for his chilling crimes.
Oskar Schröder: Luftwaffe’s top doc. Convicted but got life in the cooler instead of a dance with the hangman.
Wolfram Sievers: Director of the Ahnenerbe Institute. Convicted and executed. Guess his “research” didn’t save him from the big chill.
Some of these cold-hearted criminals actually got off scot-free:
Siegfried Ruff: Luftwaffe doc involved in the frosty fun. Acquitted faster than ice melting on a hot day.
Georg August Weltz: Another Luftwaffe doc who contributed to the cool research. Also acquitted, proving that sometimes justice is as blind as a snowstorm.
Other Notes
Mackowiak PA, Wasserman SS, Levine MM. A Critical Appraisal of 98.6°F, the Upper Limit of the Normal Body Temperature, and Other Legacies of Carl Reinhold August Wunderlich. JAMA. 1992;268(12):1578–1580. doi:10.1001/jama.1992.03490120092034 Conclusions. —Thirty-seven degrees centigrade (98.6°F) should be abandoned as a concept relevant to clinical thermometry; 37.2°C (98.9°F) in the early morning and 37.7°C (99.9°F) overall should be regarded as the upper limit of the normal oral temperature range in healthy adults aged 40 years or younger, and several of Wunderlich’s other cherished dictums should be revised.(JAMA. 1992;268:1578-1580)
Katz, Brigit. Human Body Temperature Is Getting Cooler, Study Finds –
Our average normal temperature may no longer be 98.6 degrees Fahrenheit Smithsonian Magazine January 16, 2020. Accessed March 8, 2024 Quote: “In previous studies people who found lower temperatures [in more recent times] thought the temperatures taken in the 19th century were just wrong,” study co-author Julie Parsonnet, a professor of medicine at Stanford’s School of Medicine, tells Alice Park of Time magazine. “I don’t think they were wrong; I think the temperature has gone down.” (I think she’s right about the temperature going down but I disagree on most of the whys…almost all of them.)
Protsiv, Myroslava et al. “Decreasing human body temperature in the United States since the industrial revolution.” eLife vol. 9 e49555. 7 Jan. 2020, doi:10.7554/eLife.49555 Abstract: In the US, the normal, oral temperature of adults is, on average, lower than the canonical 37°C established in the 19th century. We postulated that body temperature has decreased over time. Using measurements from three cohorts—the Union Army Veterans of the Civil War (N = 23,710; measurement years 1860–1940), the National Health and Nutrition Examination Survey I (N = 15,301; 1971–1975), and the Stanford Translational Research Integrated Database Environment (N = 150,280; 2007–2017)—we determined that mean body temperature in men and women, after adjusting for age, height, weight and, in some models date and time of day, has decreased monotonically by 0.03°C per birth decade. A similar decline within the Union Army cohort as between cohorts, makes measurement error an unlikely explanation. This substantive and continuing shift in body temperature—a marker for metabolic rate—provides a framework for understanding changes in human health and longevity over 157 years.
Basal body temperature
Main article: Basal body temperature
Basal body temperature is the lowest temperature attained by the body during rest (usually during sleep). It is generally measured immediately after awakening and before any physical activity has been undertaken, although the temperature measured at that time is somewhat higher than the true basal body temperature. In women, temperature differs at various points in the menstrual cycle, and this can be used in the long term to track ovulation both to aid conception or avoid pregnancy. This process is called fertility awareness.
Core temperature
Core temperature, also called core body temperature, is the operating temperature of an organism, specifically in deep structures of the body such as the liver, in comparison to temperatures of peripheral tissues. Core temperature is normally maintained within a narrow range so that essential enzymatic reactions can occur. Significant core temperature elevation (hyperthermia) or depression (hypothermia) over more than a brief period of time is incompatible with human life.
Hypothermia
Main article: Hypothermia
In hypothermia, body temperature drops below that required for normal metabolism and bodily functions. In humans, this is usually due to excessive exposure to cold air or water, but it can be deliberately induced as a medical treatment. Symptoms usually appear when the body’s core temperature drops by 1–2 °C (1.8–3.6 °F) below normal temperature.
Hypothermia Pathophysiology
Heat is primarily generated in muscle tissue, including the heart, and in the liver, while it is lost through the skin (90%) and lungs (10%). Heat production may be increased two- to four-fold through muscle contractions (i.e. exercise and shivering). The rate of heat loss is determined, as with any object, by convection, conduction, and radiation. The rates of these can be affected by body mass index, body surface area to volume ratios, clothing and other environmental conditions.
- Nuckton TJ, Claman DM, Goldreich D, Wendt FC, Nuckton JG (October 2000). “Hypothermia and afterdrop following open water swimming: the Alcatraz/San Francisco Swim Study”. American Journal of Emergency Medicine. 18 (6): 703–7. doi:10.1053/ajem.2000.16313. PMID 11043627.
- Hanania NA, Zimmerman JL (1999). “Accidental hypothermia”. Critical Care Clinics. 15 (2): 235–49. doi:10.1016/s0749-0704(05)70052-x. PMID 10331126.
- https://en.wikipedia.org/wiki/Hypothermia
Many changes to physiology occur as body temperatures decrease. These occur in the cardiovascular system leading to the Osborn J wave and other dysrhythmias, decreased central nervous system electrical activity, cold diuresis, and non-cardiogenic pulmonary edema.
- Marx J (2010). Rosen’s emergency medicine: concepts and clinical practice 7th edition. Philadelphia, PA: Mosby/Elsevier. pp. 1869–1870. ISBN 978-0-323-05472-0.
- https://en.wikipedia.org/wiki/Hypothermia
Research has shown that glomerular filtration rates (GFR) decrease as a result of hypothermia. In essence, hypothermia increases preglomerular vasoconstriction, thus decreasing both renal blood flow (RBF) and GFR.
- Broman M, Källskog O (1995). “The effects of hypothermia on renal function and haemodynamics in the rat”. Acta Physiologica Scandinavica. 153 (2): 179–184. doi:10.1111/j.1748-1716.1995.tb09849.x. PMID 7778458.
- Broman M, Källskog O, Kopp UC, Wolgast M (1998). “Influence of the sympathetic nervous system on renal function during hypothermia”. Acta Physiologica Scandinavica. 163 (3): 241–249. doi:10.1046/j.1365-201x.1998.00356.x. PMID 9715736.
- https://en.wikipedia.org/wiki/Hypothermia
Diagnosis
Accurate determination of core temperature often requires a special low temperature thermometer, as most clinical thermometers do not measure accurately below 34.4 °C (93.9 °F). A low temperature thermometer can be placed in the rectum, esophagus or bladder. Esophageal measurements are the most accurate and are recommended once a person is intubated. Other methods of measurement such as in the mouth, under the arm, or using an infrared ear thermometer are often not accurate.
- Brown DJ, Brugger H, Boyd J, Paal P (November 2012). “Accidental hypothermia”. The New England Journal of Medicine. 367 (20): 1930–8. doi:10.1056/NEJMra1114208. PMID 23150960. S2CID 205116341.
- McCullough L, Arora S (December 2004). “Diagnosis and treatment of hypothermia”. American Family Physician. 70 (12): 2325–32. PMID 15617296.
- https://en.wikipedia.org/wiki/Hypothermia
As a hypothermic person’s heart rate may be very slow, prolonged feeling for a pulse could be required before detecting. In 2005, the American Heart Association recommended at least 30–45 seconds to verify the absence of a pulse before initiating CPR. Others recommend a 60-second check.
- ECC Committee, Subcommittees and Task Forces of the American Heart Association (December 2005). “2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care”. Circulation. 112 (24 Suppl): IV–136. doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375. Archived from the original on March 24, 2011.
- Brown DJ, Brugger H, Boyd J, Paal P (November 2012). “Accidental hypothermia”. The New England Journal of Medicine. 367 (20): 1930–8. doi:10.1056/NEJMra1114208. PMID 23150960. S2CID 205116341
- https://en.wikipedia.org/wiki/Hypothermia
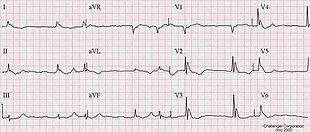
The classical ECG finding of hypothermia is the Osborn J wave. Also, ventricular fibrillation frequently occurs below 28 °C (82 °F) and asystole below 20 °C (68 °F). The Osborn J may look very similar to those of an acute ST elevation myocardial infarction. Thrombolysis as a reaction to the presence of Osborn J waves is not indicated, as it would only worsen the underlying coagulopathy caused by hypothermia.
- Hanania NA, Zimmerman JL (1999). “Accidental hypothermia”. Critical Care Clinics. 15 (2): 235–49. doi:10.1016/s0749-0704(05)70052-x. PMID 10331126.
- Marx J (2010). Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th ed.). Philadelphia: Mosby/Elsevier. p. 1862. ISBN 978-0-323-05472-0. p.1869
- https://en.wikipedia.org/wiki/Hypothermia
Nazi human experimentation
Nazi human experimentation was a series of medical experiments on prisoners by Nazi Germany in its concentration camps mainly between 1942 and 1945. There were 15,754 documented victims, of various nationalities and age groups, although the true number is believed to be more extensive. Many survived, with only a quarter of documented victims killed. Survivors generally experienced severe permanent injuries.
- Weindling, Paul; von Villiez, Anna; Loewenau, Aleksandra; Farron, Nichola (2016). “The victims of unethical human experiments and coerced research under National Socialism”. Endeavour. Elsevier BV. 40 (1): 1–6. doi:10.1016/j.endeavour.2015.10.005. ISSN 0160-9327. PMC 4822534. PMID 26749461.
- https://en.wikipedia.org/wiki/Nazi_human_experimentation#Freezing_experiments
At Auschwitz and other camps, under the direction of Eduard Wirths, selected inmates were subjected to various experiments that were designed to help German military personnel in combat situations, develop new weapons, aid in the recovery of military personnel who had been injured, and to advance Nazi racial ideology and eugenics, including the twin experiments of Josef Mengele. Aribert Heim conducted similar medical experiments at Mauthausen.
- “Nazi Medical Experimentation”. US Holocaust Memorial Museum. Retrieved 23 March 2008.
- Wachsmann, Nikolaus (2015). KL: A History of the Nazi Concentration Camps. New York, NY, United States of America: Farrar Straus & Giroux. p. 505. ISBN 978-0-374-11825-9.
- “Nazi ‘Doctor Death’ found refuge in Cairo, died in 1992”. France 24. 4 February 2009. Retrieved 16 March 2021.
- https://en.wikipedia.org/wiki/Nazi_human_experimentation#Freezing_experiments
After the war, these crimes were tried at what became known as the Doctors’ Trial, and revulsion at the abuses perpetrated led to the development of the Nuremberg Code of medical ethics. The Nazi physicians in the Doctors’ Trial argued that military necessity justified their experiments and compared their victims to collateral damage from Allied bombings.
Experiments
The table of contents of a document from the Subsequent Nuremberg trials prosecution includes titles of the sections that document medical experiments revolving around food, seawater, epidemic jaundice, sulfanilamide, blood coagulation and phlegmon. According to the indictments at the subsequent Nuremberg Trials, these experiments included the following:
Freezing experiments

In 1941, the Luftwaffe conducted experiments with the intent of discovering means to prevent and treat hypothermia. There were 360 to 400 experiments and 280 to 300 victims, indicating that some victims suffered more than one experiment.
- Berger, Robert L. (May 1990). “Nazi Science — the Dachau Hypothermia Experiments”. New England Journal of Medicine. 322 (20): 1435–40. doi:10.1056/NEJM199005173222006. PMID 2184357
- “Nuremberg – Document Viewer – Table of contents for prosecution document book 8, concerning medical experiments”. nuremberg.law.harvard.edu. Retrieved 2017-04-14.
- “Medical Experiment”. Jewish Virtual Library. Retrieved 23 March 2008.
- “The Doctors Trial: The Medical Case of the Subsequent Nuremberg Proceedings”. United States Holocaust Memorial Museum. Archived from the original on 20 April 2008. Retrieved 23 March 2008.
- https://en.wikipedia.org/wiki/Nazi_human_experimentation#Freezing_experiments

