Urokinase (and Porta Johns?)
Recycling Fever Reaches New Lows
“Utica, Michigan – Realising it is flushing potential profits down the drain, an enterprising young company has come up with a way to trap medically powerful proteins from urine. Enzymes of America has designed a special filter that collects important urine proteins, and these filters have been installed in all of the men’s urinals in the 10,000 portable outhouses owned by the Porta-John company, a subsidiary of Enzymes of America. Urine is known to contain minute amounts of proteins made by the body, including medically important ones such as growth hormone and insulin. There is a $500-million-a-year market for these kinds of urine ingredients. This summer, Enzymes of America plans to market its first major urine product called urokinase, an enzyme that dissolves blood clots and is used to treat victims of heart attacks. The company has contracts to supply the urine enzyme to Sandoz, Merrell Dow and other major pharmaceutical companies. Ironically, this enterprise evolved from Porta-John’s attempt to get rid of urine proteins-a major source of odour in portable toilets. When the president of Porta-John began consulting with scientists about a urine filtration system, one told him he was sitting on a gold mine. The idea of recycling urine is not new, however. ‘We thought about this,’ says Ian Whitcome of Amgen, a Los Angeles biotechnology firm, ‘but realised we’d need thousands and thousands of litres of urine.’ Porta-John and Enzymes of America solved that problem. The 14 million gallons flowing annually into Porta-John’s privies contain about four-and-a-half pounds of urokinase alone. That’s enough to unclog 260,000 coronary arteries.” (Hippocrates magazine, May/June 1988)
John F. Kelly quoting Hippocrates magazine? It is unclear to me what this is exactly. I did not find it in a table of contents for that magazine. It is copied in similar format on several websites. Mysteries for another day. His article is interesting in any case and now we will head to Wikipedia to look up Urokinase because that’s what we do.
I am disappointed there is no Wikipedia page for Porta John or the other things and individuals involved with such a (rags to riches?) enterprise. If you believe the stories they started out with a couple of wooden toilets and a truck and ended up making billions. There is some interesting history involving not only urokinase, and “pharmaceuticals made from human waste” but a legal dispute with the estate of Johnny Carson over use of the phrase “Here’s Johnny” for toilet ads and another with the United States over subterfuge or unpaid taxes or something. I think it is odd they have no Wikipedia pages.
From Wikipedia, the free encyclopedia
Urokinase, also known as urokinase-type plasminogen activator (uPA), is a serine protease present in humans and other animals. The human urokinase protein was discovered, but not named, by McFarlane and Pilling in 1947.
- Degryse B (1 June 2011). “The urokinase receptor system as strategic therapeutic target: challenges for the 21st century”. Current Pharmaceutical Design. 17 (19): 1872–1873. doi:10.2174/138161211796718161. PMID 21711231.
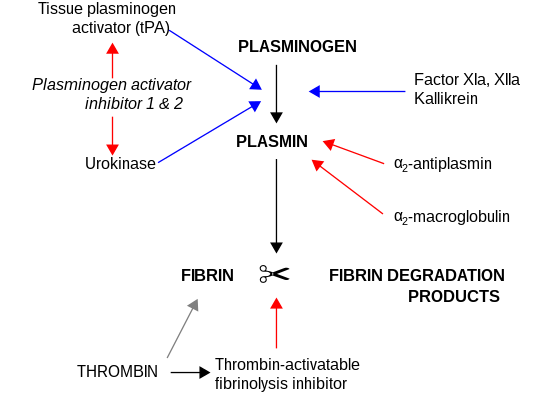
Urokinase was originally isolated from human urine, and it is also present in the blood and in the extracellular matrix of many tissues. The primary physiological substrate of this enzyme is plasminogen, which is an inactive form (zymogen) of the serine protease plasmin. Activation of plasmin triggers a proteolytic cascade that, depending on the physiological environment, participates in thrombolysis or extracellular matrix degradation. This cascade had been involved in vascular diseases and cancer progression.
- Tang L, Han X (March 2013). “The urokinase plasminogen activator system in breast cancer invasion and metastasis”. Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie. 67 (2): 179–182. doi:10.1016/j.biopha.2012.10.003.
Urokinase is encoded in humans by the PLAU gene, which stands for “plasminogen activator, urokinase”. The same symbol represents the gene in other animal species.
- Nagai M, Hiramatsu R, Kanéda T, Hayasuke N, Arimura H, Nishida M, Suyama T (Dec 1985). “Molecular cloning of cDNA coding for human preprourokinase”. Gene. 36 (1–2): 183–188. doi:10.1016/0378-1119(85)90084-8. PMID 2415429.
Structure
Urokinase is a 411-residue protein, consisting of three domains: the serine protease domain (consisting of residues 159-411), the kringle domain (consisting of residues 50-131), and the EGF-like domain (consisting of residues 1-49). The kringle domain and the serine protease domain are connected by an interdomain linker or connecting peptide (consisting of residues 132-158). Urokinase is synthesized as a zymogen form (prourokinase or single-chain urokinase), and is activated by proteolytic cleavage between Lys158 and Ile159. The two resulting chains are kept together by a disulfide bond between Cys148 and Cys279.
- Vincenza Carriero M, Franco P, Vocca I, Alfano D, Longanesi-Cattani I, Bifulco K, et al. (January 2009). “Structure, function and antagonists of urokinase-type plasminogen activator”. Frontiers in Bioscience. 14 (10): 3782–3794. doi:10.2741/3488. PMID 19273310.
Interaction partners
The most important inhibitors of urokinase are the serpins plasminogen activator inhibitor-1 (PAI-1) and plasminogen activator inhibitor-2 (PAI-2), which inhibit the protease activity irreversibly. In the extracellular matrix, urokinase is tethered to the cell membrane by its interaction to the urokinase receptor.
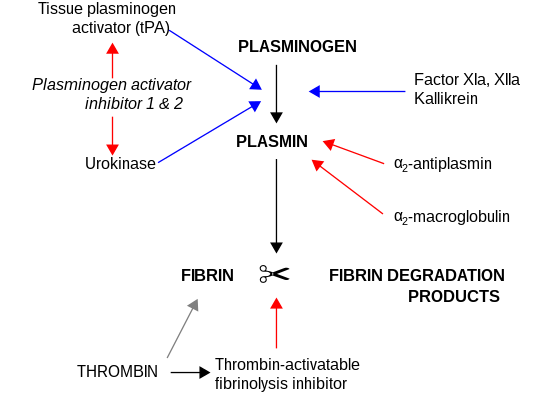
Fibrinolysis (simplified). Blue arrows denote stimulation, and red arrows inhibition.
uPa also interacts with protein C inhibitor.
- Geiger M, Huber K, Wojta J, Stingl L, Espana F, Griffin JH, Binder BR (August 1989). “Complex formation between urokinase and plasma protein C inhibitor in vitro and in vivo”. Blood. 74 (2): 722–728. doi:10.1182/blood.V74.2.722.722. PMID 2752144.
- España F, Berrettini M, Griffin JH (August 1989). “Purification and characterization of plasma protein C inhibitor”. Thrombosis Research. 55 (3): 369–384. doi:10.1016/0049-3848(89)90069-8. PMID 2551064.
Urokinase and cancer
Elevated expression levels of urokinase and several other components of the plasminogen activation system are found to be correlated with tumor malignancy. It is believed that the tissue degradation following plasminogen activation facilitates tissue invasion and, thus, contributes to metastasis. Urokinase-type plasminogen activator (uPA) is more commonly associated with cancer progression than tissue plasminogen activator (tPA). This makes uPA an attractive drug target, and, so, inhibitors have been sought to be used as anticancer agents. However, incompatibilities between the human and murine systems hamper clinical evaluation of these agents. Moreover, urokinase is used by normal cells for tissue remodeling and vessel growth, which necessitates distinguishing cancer-associated urokinase features for specific targeting.
- Madunić J (December 2018). “The Urokinase Plasminogen Activator System in Human Cancers: An Overview of Its Prognostic and Predictive Role”. Thrombosis and Haemostasis. 118 (12): 2020–2036. doi:10.1055/s-0038-1675399. PMID 30419600.
- Mahmood N, Mihalcioiu C, Rabbani SA (2018). “Multifaceted Role of the Urokinase-Type Plasminogen Activator (uPA) and Its Receptor (uPAR): Diagnostic, Prognostic, and Therapeutic Applications”. Frontiers in Oncology. 8: 24. doi:10.3389/fonc.2018.00024. PMC 5816037. PMID 29484286.
- Jankun J, Skrzypczak-Jankun E (July 1999). “Molecular basis of specific inhibition of urokinase plasminogen activator by amiloride”. Cancer Biochemistry Biophysics. 17 (1–2): 109–123. PMID 10738907.
- Matthews H, Ranson M, Kelso MJ (November 2011). “Anti-tumour/metastasis effects of the potassium-sparing diuretic amiloride: an orally active anti-cancer drug waiting for its call-of-duty?”. International Journal of Cancer. 129 (9): 2051–2061. doi:10.1002/ijc.26156. PMID 21544803. S2CID 205943879.
uPA breakdown of the extracellular matrix is crucial for initiating the angiogenesis which is associated with cancer growth. uPA antigen is elevated in breast cancer tissue, which correlates with poor prognosis in breast cancer patients. For this reason, uPA can be used as a diagnostic biomarker in breast cancer.
- Mahmood N, Mihalcioiu C, Rabbani SA (2018). “Multifaceted Role of the Urokinase-Type Plasminogen Activator (uPA) and Its Receptor (uPAR): Diagnostic, Prognostic, and Therapeutic Applications”. Frontiers in Oncology. 8: 24. doi:10.3389/fonc.2018.00024. PMC 5816037. PMID 29484286.
Through its interaction with the urokinase receptor, urokinase affects several other aspects of cancer biology such as cell adhesion, migration, and cellular mitotic pathways.
As of December 7, 2012, Mesupron (upamostat), a small molecule serine protease inhibitor developed by the WILEX pharmaceutical company, has completed phase II trials. Mesupron appears to be safe when combined with chemotherapeutic drug Capecitabine for the progression-free survival in human breast cancer.
- Gemcitabine With or Without WX-671 in Treating Patients With Locally Advanced Pancreatic Cancer That Cannot Be Removed By Surgery”. ClinicalTrials.gov. 28 March 2012.
- “Fox Chase Cancer Center : New Small Molecule Inhibitor Could be a Safe and First-Line Treatment for Metastatic Breast Cancer”. Press Release. Temple University Health System.
Clinical applications
Urokinase is effective for the restoration of flow to intravenous catheters blocked by clotted blood or fibrin (catheter clearance). Catheters are used extensively to administer treatments to patients for such purposes as dialysis, nutrition, antibiotic treatment and cancer treatment. Approximately 25% of catheters become blocked, meaning that affected patients cannot receive treatment until the catheter has been cleared or replaced. Urokinase is also used clinically as a thrombolytic agent in the treatment of severe or massive deep venous thrombosis, peripheral arterial occlusive disease, pulmonary embolism, acute myocardial infarction (AMI, heart attack), and occluded dialysis cannulas (catheter clearance). It is also administered intrapleurally to improve the drainage of complicated pleural effusions and empyemas. Urokinase is marketed as Kinlytic (formerly Abbokinase) and competes with recombinant tissue plasminogen activator (e.g., alteplase) as a thrombolytic drug.
All plasminogen activators (urokinase, tPA) catalyze the production of plasmin, which in turn leads to the breakdown of the fibrin mesh structure in blood clots. While there are commonalities in the mode of action for urokinase and tPA, urokinase has some advantages for treatment of peripheral clots (Pulmonary Embolism, Deep Vein Thrombosis, Peripheral arterial occlusive disease).
Unlike tPA, which is activated by binding to the fibrin within clots, urokinase is not sequestered by fibrin and therefore does not specifically attack hemostatic clots. This makes urokinase less likely to break down such hemostatic clots that are essential for ongoing blood vessel repair throughout the body. Dissolution of these “good” clots can lead to serious adverse events through hemorrhagic bleeding. Years of clinical study have confirmed the safety advantage of using urokinase. Consequently, urokinase has been preferentially used in deep venous thrombosis and peripheral arterial occlusive disease where it is administered directly to the site of the clot while tPA is preferred in AMI where peripheral bleeding is a secondary consideration.
- Ouriel K, Gray B, Clair DG, Olin J (March 2000). “Complications associated with the use of urokinase and recombinant tissue plasminogen activator for catheter-directed peripheral arterial and venous thrombolysis”. Journal of Vascular and Interventional Radiology. 11 (3): 295–298. doi:10.1016/S1051-0443(07)61420-1. PMID 10735422.
- Cinà CS, Goh RH, Chan J, Kenny B, Evans G, Rawlinson J, Gill G (November 1999). “Intraarterial catheter-directed thrombolysis: urokinase versus tissue plasminogen activator”. Annals of Vascular Surgery. 13 (6): 571–575. doi:10.1007/s100169900300. PMID 10541608. S2CID 470599.
A revolutionary method for the production of urokinase was patented by Evelyn Nicol in 1976 (U.S. Patent No. 3,930,944). Nicol was believed to be the first African American woman to receive a molecular biology patent.
- “Evelyn Nicol 1930 – 2020 – Obituary”. www.legacy.com. Retrieved 2020-08-28.
Evelyn Nicol has a Wikipedia page and interesting links to folks that keep popping up all over everything. Briefly, and from her Wikipedia page,
“Nicol was offered a scholarship at Tuskegee University to study Home Economics. She moved to Alabama in 1949 to attend university, but she chose to study Mathematics and Chemistry instead of Home Economics. She funded her studies by working two jobs. Nicol graduated at the top of her class in 1953 with a degree in Chemistry and Mathematics, and earned the Beta Kappa Chi and Alpha Kappa Mu honors. From 1953 to 1955, Nicol worked as a research assistant for the Salk Polio Project of the Carver Research Foundation. Under the supervision of Dr. Russel W. Brown, she worked on developing the first polio vaccine using HeLa cell cultures.
- HeLa is an immortalized cell line used in scientific research. It is the oldest and most commonly used human cell line. The line is derived from cervical cancer cells taken on February 8, 1951, named after Henrietta Lacks, (Oprah Winfrey played her daughter in the movie The Immortal Life of Henrietta Lacks). The cell line was found to be remarkably durable and prolific, which allows it to be used extensively in scientific study. There are many strains of HeLa cells as they continue to mutate in cell cultures, but all HeLa cells are descended from the same tumor cells removed from Lacks. In 1965, Henry Harris and John Watkins created the first human-animal hybrid by fusing HeLa cells with mouse embryo cells. In the 1960s, HeLa cells were sent on the Soviet satellite Sputnik-6 and human space missions to determine the long term effects of space travel on living cells and tissue. Scientists discovered that HeLa cells divided even more quickly in zero gravity. HeLa cells were used by Jonas Salk to test the first polio vaccine in the 1950s. They were observed to be easily infected by poliomyelitis, causing infected cells to die. This made HeLa cells highly desirable for polio vaccine testing since results could be easily obtained. A large volume of HeLa cells were needed for the testing of Salk’s polio vaccine, prompting the National Foundation for Infantile Paralysis (NFIP) to find a facility capable of mass-producing HeLa cells. In the spring of 1953, a cell culture factory was established at Tuskegee University to supply Salk and other labs with HeLa cells. Less than a year later, Salk’s vaccine was ready for human trials. Lots more available at Wikipedia and elsewhere.
Nicol then joined the Cleveland City Hospital, working with Frederick C. Robbins and John F. Enders.
- Frederick C. Robbins (pediatrician and virologist, received the Nobel Prize in Physiology or Medicine in 1954 along with John Franklin Enders and Thomas Huckle Weller, for breakthrough work in isolating and growing the poliovirus in tissue culture, paving the way for vaccines developed by Jonas Salk and Albert Sabin).
- John F. Enders (mentioned above in the Nobel Prize business, Wikipedia says he is called the Father of Modern Vaccines mentioning polio and measles).
There, she was the first person to successfully isolate the herpes zoster virus, which causes shingles, using amniotic cells in tissue culture. Nicol was headhunted by Rand Development Corporation, where she worked on isolating the leukemia agent. During this time, Nicol also worked for the University of Kansas Medical Centre, and the Michael Reese Hospital. Nicol then joined Abbott Laboratories as a research assistant in 1962. There, she faced discrimination from her white colleagues, who would take credit for results and sabotage her work. On 6 January 1976, Nicol patented a new technique to produce urokinase (U.S. Patent No. 3,930,944), an enzyme used to dissolve blood clots. She was one of the few African American women to be awarded a patent in molecular biology at that time. Among her many achievements while working at Abbott, Nicol successfully developed a test for toxoplasmosis in pregnant women, and an interferon assay. In 1985, Nicol was recruited by Baxter Pharmaceuticals. Within their hepatitis research and development group, known as Pandex, Nicol led the retrovirology division, which produced testing kits for blood-borne diseases such as HIV. Two blind studies funded by Abbott Pharmaceuticals determined that the testing kits produced under Nicol’s leadership were the best available. At the age of 89, Nicol was hospitalized for a stroke, and was diagnosed with COVID-19. She died from complications of the virus in May 2020.
Society and culture
The presence of a fibrinolytic enzyme in human urine was reported in 1947, without a name given for such an enzyme behind its effect.
- Macfarlane RG, Pilling J (June 1947). “Fibrinolytic activity of normal urine”. Nature. 159 (4049):779. Bibcode:1947Natur.159Q.779M. doi:10.1038/159779a0. PMID 20241608. S2CID 4125748.
In 1952 a purified form of the enzyme was extracted from human urine and named “urokinase” for “urinary kinase”. The full text for this article is lost, and the only citation points to the abstract of a list of papers read at a conference in the same journal.
- Sobel GW, Mohler SR, Jones NW, Dowdy ABC, Guest MM. Urokinase: an activator of plasma profibrinolysin extracted from urine. Am J Physiol 1952; 171: 768-69.
- “Abstracts of Papers Read”. American Journal of Physiology. Legacy Content. 171 (3): 704–781. 30 November 1952. doi:10.1152/ajplegacy.1952.171.3.704.
Normal human and dog urine contains fibrinolysin (plasmin) and a potent activator of profibrinolysin (plasminogen). The activator, which we have designated urokinase, can be concentrated and partially purified by acetone or alcohol fractionation methods.
A few other papers on the purification were published independently around the same time. By 1960, it was still unclear whether the activation of plasminogen has anything to do with a protease, but a kinase is thought to play a role regardless.
- Celander DR, Guest MM (August 1960). “The biochemistry and physiology of urokinase”. The American Journal of Cardiology. 6 (2): 409–419. doi:10.1016/0002-9149(60)90333-7. PMID 13808740.
References
- GRCh38: Ensembl release 89: ENSG00000122861 – Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000021822 – Ensembl, May 2017
- “Human PubMed Reference:”. National Center for Biotechnology Information, U.S. National Library of Medicine.
- “Mouse PubMed Reference:”. National Center for Biotechnology Information, U.S. National Library of Medicine.
- Degryse B (1 June 2011). “The urokinase receptor system as strategic therapeutic target: challenges for the 21st century”. Current Pharmaceutical Design. 17 (19): 1872–1873. doi:10.2174/138161211796718161. PMID 21711231.
- Tang L, Han X (March 2013). “The urokinase plasminogen activator system in breast cancer invasion and metastasis”. Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie. 67 (2): 179–182. doi:10.1016/j.biopha.2012.10.003. PMID 23201006.
- Nagai M, Hiramatsu R, Kanéda T, Hayasuke N, Arimura H, Nishida M, Suyama T (Dec 1985). “Molecular cloning of cDNA coding for human preprourokinase”. Gene. 36 (1–2): 183–188. doi:10.1016/0378-1119(85)90084-8. PMID 2415429.
- “Entrez Gene: PLAU plasminogen activator, urokinase”.
- Vincenza Carriero M, Franco P, Vocca I, Alfano D, Longanesi-Cattani I, Bifulco K, et al. (January 2009). “Structure, function and antagonists of urokinase-type plasminogen activator”. Frontiers in Bioscience. 14 (10): 3782–3794. doi:10.2741/3488. PMID 19273310.
- Geiger M, Huber K, Wojta J, Stingl L, Espana F, Griffin JH, Binder BR (August 1989). “Complex formation between urokinase and plasma protein C inhibitor in vitro and in vivo”. Blood. 74 (2): 722–728. doi:10.1182/blood.V74.2.722.722. PMID 2752144.
- España F, Berrettini M, Griffin JH (August 1989). “Purification and characterization of plasma protein C inhibitor”. Thrombosis Research. 55 (3): 369–384. doi:10.1016/0049-3848(89)90069-8. PMID 2551064.
- Madunić J (December 2018). “The Urokinase Plasminogen Activator System in Human Cancers: An Overview of Its Prognostic and Predictive Role”. Thrombosis and Haemostasis. 118 (12): 2020–2036. doi:10.1055/s-0038-1675399. PMID 30419600.
- Mahmood N, Mihalcioiu C, Rabbani SA (2018). “Multifaceted Role of the Urokinase-Type Plasminogen Activator (uPA) and Its Receptor (uPAR): Diagnostic, Prognostic, and Therapeutic Applications”. Frontiers in Oncology. 8: 24. doi:10.3389/fonc.2018.00024. PMC 5816037. PMID 29484286.
- Jankun J, Skrzypczak-Jankun E (July 1999). “Molecular basis of specific inhibition of urokinase plasminogen activator by amiloride”. Cancer Biochemistry Biophysics. 17 (1–2): 109–123. PMID 10738907.
- Matthews H, Ranson M, Kelso MJ (November 2011). “Anti-tumour/metastasis effects of the potassium-sparing diuretic amiloride: an orally active anti-cancer drug waiting for its call-of-duty?”. International Journal of Cancer. 129 (9): 2051–2061. doi:10.1002/ijc.26156. PMID 21544803. S2CID 205943879.
- “Gemcitabine With or Without WX-671 in Treating Patients With Locally Advanced Pancreatic Cancer That Cannot Be Removed By Surgery”. ClinicalTrials.gov. 28 March 2012.
- “Fox Chase Cancer Center : New Small Molecule Inhibitor Could be a Safe and First-Line Treatment for Metastatic Breast Cancer”. Press Release. Temple University Health System.
- Ouriel K, Gray B, Clair DG, Olin J (March 2000). “Complications associated with the use of urokinase and recombinant tissue plasminogen activator for catheter-directed peripheral arterial and venous thrombolysis”. Journal of Vascular and Interventional Radiology. 11 (3): 295–298. doi:10.1016/S1051-0443(07)61420-1. PMID 10735422.
- Cinà CS, Goh RH, Chan J, Kenny B, Evans G, Rawlinson J, Gill G (November 1999). “Intraarterial catheter-directed thrombolysis: urokinase versus tissue plasminogen activator”. Annals of Vascular Surgery. 13 (6): 571–575. doi:10.1007/s100169900300. PMID 10541608. S2CID 470599.
- “Evelyn Nicol 1930 – 2020 – Obituary”. www.legacy.com. Retrieved 2020-08-28.
- Macfarlane RG, Pilling J (June 1947). “Fibrinolytic activity of normal urine”. Nature. 159 (4049): 779. Bibcode:1947Natur.159Q.779M. doi:10.1038/159779a0. PMID 20241608. S2CID 4125748.
- Sobel GW, Mohler SR, Jones NW, Dowdy ABC, Guest MM. Urokinase: an activator of plasma profibrinolysin extracted from urine. Am J Physiol 1952; 171: 768-69.
- “Abstracts of Papers Read”. American Journal of Physiology. Legacy Content. 171 (3): 704–781. 30 November 1952. doi:10.1152/ajplegacy.1952.171.3.704.
Normal human and dog urine contains fibrinolysin (plasmin) and a potent activator of profibrinolysin (plasminogen). The activator, which we have designated urokinase, can be concentrated and partially purified by acetone or alcohol fractionation methods.
- Celander DR, Guest MM (August 1960). “The biochemistry and physiology of urokinase”. The American Journal of Cardiology. 6 (2): 409–419. doi:10.1016/0002-9149(60)90333-7. PMID 13808740.
Further reading
- Ploug M, Gårdsvoll H, Jørgensen TJ, Lønborg Hansen L, Danø K (April 2002). “Structural analysis of the interaction between urokinase-type plasminogen activator and its receptor: a potential target for anti-invasive cancer therapy”. Biochemical Society Transactions. 30 (2): 177–183. doi:10.1042/BST0300177. PMID 12023847.
- Alfano M, Sidenius N, Blasi F, Poli G (November 2003). “The role of urokinase-type plasminogen activator (uPA)/uPA receptor in HIV-1 infection”. Journal of Leukocyte Biology. 74 (5): 750–756. doi:10.1189/jlb.0403176. PMID 12960238. S2CID 8526093.
- Harbeck N, Kates RE, Gauger K, Willems A, Kiechle M, Magdolen V, Schmitt M (March 2004). “Urokinase-type plasminogen activator (uPA) and its inhibitor PAI-I: novel tumor-derived factors with a high prognostic and predictive impact in breast cancer”. Thrombosis and Haemostasis. 91 (3): 450–456. doi:10.1160/TH03-12-0798. PMID 14983219. S2CID 19904733.
- Gilabert-Estelles J, Ramon LA, España F, Gilabert J, Castello R, Estelles A (2006). “Expression of the fibrinolytic components in endometriosis”. Pathophysiology of Haemostasis and Thrombosis. 35 (1–2): 136–140. doi:10.1159/000093556. PMID 16855359. S2CID 29270171.
External links
- Overview of all the structural information available in the PDB for UniProt: P00749 (Human Urokinase-type plasminogen activator) at the PDBe-KB.
- Overview of all the structural information available in the PDB for UniProt: P06869 (Mouse Urokinase-type plasminogen activator) at the PDBe-KB.
| PDB gallery |
|---|


Leave a Reply